Mucous membrane pemphigoid is a rare ocular surface disease usually due to an autoimmune reaction of the patient’s body to the cells in the conjunctiva ,and eventually the cornea, plus other mucous membranes.
Call Us: 215-928-3180
Mucous membrane pemphigoid is a rare ocular surface disease usually due to an autoimmune reaction of the patient’s body to the cells in the conjunctiva ,and eventually the cornea, plus other mucous membranes.
Call Us: 215-928-3180
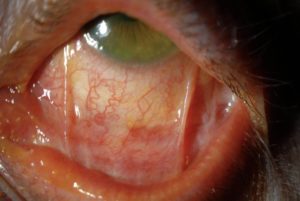
Mucous membrane pemphigoid (MMP), often called ocular cicatricial pemphigoid (OCP), is a rare ocular surface disease usually due to an autoimmune reaction of the patient’s body to the cells in the conjunctiva and eventually the cornea.
 It often begins with the feeling of dryness and irritation. Over months to years, the symptoms can worsen and vision can be affected.
It often begins with the feeling of dryness and irritation. Over months to years, the symptoms can worsen and vision can be affected.
The diagnosis is usually made during an office examination and can sometimes be confirmed by a small biopsy of the conjunctiva.
Treatment of MMP/OCP generally involves eye lubrication and oral anti-inflammatory medications. MMP/OCP can often be controlled with treatment but some patients get progressively worse despite aggressive management.
Mucous membrane pemphigoid (MMP), often called ocular cicatricial pemphigoid (OCP), is a rare ocular surface disease usually due to an autoimmune reaction of the patient’s body to the cells in the conjunctiva and eventually the cornea, plus other mucous membranes. It is generally progressive without (and occasionally even with) treatment and can cause permanent conjunctival and corneal scarring.
It often begins with the feeling of dryness, irritation, grittiness, sandy sensation in the eyes, but symptoms can also include redness, mucous discharge, fluctuation of vision, contact lens intolerance. Over months to years, the symptoms can worsen and vision can be affected, rarely leading to blindness. Can develop ulcerations of other mucous membranes including the mouth.
Typically autoimmune but occasionally caused by eye medications.
Advancing age.
Dry eyes, conjunctival scarring, corneal abrasions, corneal infections, corneal scarring, corneal thinning, corneal perforation.
The diagnosis can usually be made during a slit lamp examination with special dyes such as fluorescein and lissamine green. Ancillary testing includes measurement of tear production (Schirmer’s test). The diagnosis of MMP/OCP may be confirmed by a small biopsy of the conjunctiva sent for special stains.
Treatment of MMP/OCP generally involves eye lubrication and oral anti-inflammatory medications, such as steroids, mycophenolate mofetil and methotrexate. MMP/OCP can often be controlled with treatment but some patients get progressively worse despite aggressive management. If the eyelashes are turned in due to eyelid scarring, corrective eyelid surgery may be required. Rarely, mucous membrane grafting or an artificial corneal transplant (keratoprosthesis) can be performed to attempt to improve the vision. Referral to other specialists to manage systemic complications of MMP/OCP may be warranted.
Periodic eye examinations are recommended to monitor the condition. If systemic immunosuppressants are used, routine monitoring is required.
