KERATOCONUS
Keratoconus is a condition in which the cornea (the clear covering of the colored iris and black pupil) becomes protruded and irregular, affecting vision.
Call Us: 215-928-3180
Keratoconus is a condition in which the cornea (the clear covering of the colored iris and black pupil) becomes protruded and irregular, affecting vision.
Call Us: 215-928-3180
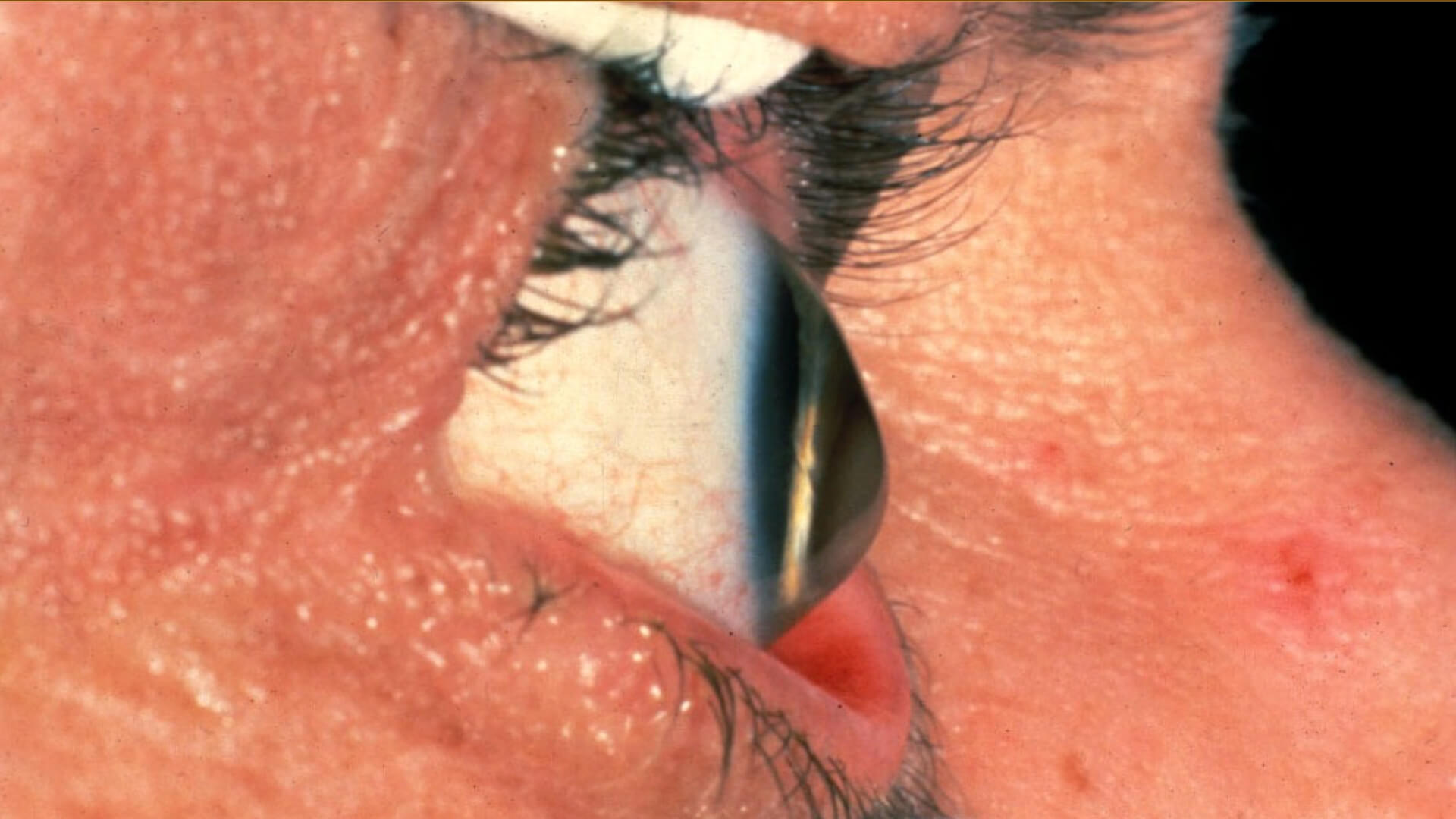
Keratoconus is a condition in which the cornea (the clear covering of the colored iris and black pupil) becomes protruded and irregular, affecting vision. It typically develops during teenage or young adulthood years, but can occur later. The cause is unknown, but eye rubbing is thought to be a factor in many patients. Occasionally keratoconus runs in families.
Initially, keratoconus causes changes in vision requiring frequent prescription updates for your eyeglasses. Later it may worsen and require contact lenses to improve vision. Soft toric lenses, rigid gas permeable lenses, piggyback, hybrid (e.g. Synergeyes), or scleral (e.g. PROSE) lenses may be used. In some patients, contact lenses do not provide good, comfortable vision, and surgery may be an option. Intacs (plastic corneal inserts) may be an option for some patients with moderate keratoconus. Corneal transplantation can be very successful for contact lens intolerant patients with keratoconus. Progressive keratoconus, or alternatively eyes that develop progressive thinning and protrusion after refractive surgery such as LASIK, may be treatable with corneal crosslinking (CXL).
CXL is a procedure that was developed in Europe over 15 years ago, used widely around the world for over 10 years and FDA approved in the US in 2016. We at Wills were involved in some of the FDA trials for CXL. The goal of the CXL procedure is to prevent progression of the condition. It is 90-95% successful in stopping progression, but there is a small chance (~1%) of a complication such as poor healing, scarring, infection, corneal swelling and decreased vision. Ask your doctor if you may be a candidate for CXL.
Keratoconus is a condition in which the cornea (the clear covering of the colored iris and black pupil) becomes protruded and irregular, affecting vision. It typically develops during teenage or young adulthood years, but can occur later. It tends to progress until the 30’s or 40’s and then tends to stabilize.
Blurred vision, usually one eye worse the to the eye. It often causes changes in vision requiring frequent glasses prescription changes, which clear the vision initially but later don’t help the vision as much.
The cause is unknown, but eye rubbing is thought to be a factor in many patients. Occasionally keratoconus runs in families.
EYE RUBBING
Cornea scarring can develop in severe cases. Acute corneal hydrops can develop in advanced cases. This is a condition where the membrane on the back layer of the cornea (Descemet’s membrane) tears and allows fluid to build up in the cornea causing pain and poor vision.
The diagnosis can usually be made during a slit lamp examination. Ancillary testing includes corneal curvature and thickness mapping (corneal topography and tomography) and measurement of the corneal thickness (pachymetry). Anterior segment optical coherence tomography (AS-OCT) may be helpful in some cases.
Mild cases may just require routine observation and mapping with or without a new glasses prescription. Later it may worsen, requiring contact lenses to improve vision. Soft toric lenses, rigid gas permeable lenses, piggyback, hybrid (e.g. Synergeyes), or scleral (e.g. PROSE) lenses may be used. In some patients, contact lenses do not provide good, comfortable vision, and surgery may be an option. Intacs (plastic corneal inserts) may be an option for some patients with moderate keratoconus. Corneal transplantation (either partial thickness or full thickness) can be very successful for contact lens intolerant patients with keratoconus.
Progressive keratoconus, or alternatively eyes that develop progressive thinning and protrusion after refractive surgery such as LASIK, may be treatable with corneal crosslinking (CXL).
Acute corneal hydrops is initially managed with medications and usually resolves on its own over weeks to months, depending on its severity. Rarely, surgery may be required for hydrops.
NO eye rubbing!! Routine eye examinations are recommended to monitor the condition. If progression of the condition is noted, corneal crosslinking should be considered. Corneal crosslinking is not indicated in eyes with significant corneal scarring or significant corneal thinning.
