Glaucoma Tube Shunts
Glaucoma tube shunt surgery may be needed to lower eye pressure in patients when medications, laser, or other surgery has not worked.
Call Us: 215-928-3197
Glaucoma tube shunt surgery may be needed to lower eye pressure in patients when medications, laser, or other surgery has not worked.
Call Us: 215-928-3197
Glaucoma tube shunt surgery may be needed to lower eye pressure in patients when medications, laser, or other surgery has not worked.
This is an outpatient procedure in the operating room. You will receive ‘twilight’ anesthesia allowing you to be comfortable for the procedure. After eye drops are put in the eye and after the eye is numbed and cleaned, a sterile drape will be put over your face and body and will leave only your eye uncovered. Your eye will be held open by a small spring so you do not have to worry about blinking during the surgery. The anesthesia team will give you sedating medications to keep you comfortable.
You may see bright lights during the surgery, but should not feel any pain. You will be discharged with a clear plastic shield with or without a patch over the operated eye. An adult will need to drive you home since you received sedating medications.
Most patients will be asked to use a steroid and antibiotic eye drops to help reduce inflammation and prevent infections. Your doctor will check your eye at each visit and may change the eye drop instructions depending on how your eye is doing. You will see your doctor the first day after surgery, about a week later, and a few weeks after that. Depending on how your eye heals, additional or fewer visits may be needed.
The first few days after surgery, vision may be worse than it was before surgery. This will improve over 1-2 weeks, although it can sometimes take longer. The vision in your other eye will not be affected, and may be depended on for vision during the recovery period (if it has vision). Depending on your job and your other eye, you should be able to return to work within a few days to a few weeks. Limitations in physical activities at work may be needed.
After surgery, your eye may be sore, and it may feel like there is something in it, like an eyelash. The drops may burn when you put them in, and your eye may water or tear a lot. These symptoms are common but usually are mild, and improve for most people after 1-2 days. Tylenol (acetaminophen) is a good option unless you are unable to take this medication. If your eye has severe pain or sudden worsening pain or vision after surgery, please call our office or on call physician immediately.
You will be given detailed instructions after your surgery that are specific to your eye’s needs. In general, the following guidelines apply:
There are no restrictions in reading, watching TV, using your phone, tablet device, computer, etc, but your eyes may tire more easily during these activities.
The simple answer is no. Any vision that is already lost before surgery will not return. Tube shunt surgery only lowers your eye pressure. By lowering the eye pressure, the goal is to either stop or slow down your loss of vision. Most people will need some glaucoma eye drops to keep their pressure under control. In some cases, people may take fewer eye drops than prior to surgery. The need for eye drops after tube shunt surgery varies greatly and is determined by your type of glaucoma and the rate it is progressing.
The tube shunt device is made of a tube and plate that are positioned under the conjunctiva (thin superficial eye tissue). The tube is carefully inserted into the front chamber of the eye, often just in front of the iris (the colored part of the eye). The fluid drains through the tube, into the area around the back end of the plate. The fluid collects here and is drained through the eye’s natural drainage system. One cannot feel the implant and it is usually not visible unless one lifts the eyelid or opens the eye very widely.
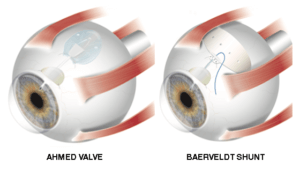
What types of shunts are available?
The Ahmed valve and Baerveldt shunt are two options. The Ahmed shunt tends to work immediately whereas the Baerveldt may take 4-6 weeks to see full effect. Your doctor will determine which tube shunt is more appropriate for your eye, as there are various differences.
All eye surgery has some risks. Any operation is not done unless the benefits outweigh the risks. Risks include, but are not limited to, bleeding, infection, hypotony (pressure that is too low), scarring, swelling, retinal detachment, droopy eyelid, double vision, loss of vision, or even loss of the eye. Sometimes the tube fails and you may need additional surgery. In general, many of the risks are not common, however you may want to discuss the benefits and risks with your surgeon should you have any further questions. All surgery has the possible need for another operation.
