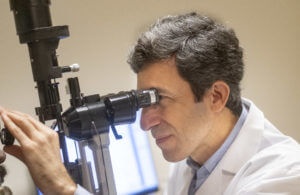
JONATHAN S. MYERS, MD
Chief, Glaucoma Service
Tips to be Prepared
After you have been checked in at the front desk -
A technician will bring you into the exam room and will ask questions about your eye history, as well as any troubles you are having. You will be asked about:
- Your eye pressure: what range it usually runs in and the highest eye pressure you can recall having for each eye.
- Eye drops you are currently taking. As well as if you are allergic/intolerant to any drops, and if any drops may not have worked for you in the past.
- Any eye surgeries and laser procedures performed in the past.
- Your prior medical records.
- Oral and other systemic medications you are taking.
- Your family history – if anyone has/had glaucoma in your family, and whether their vision was affected.
- Smoking / alcohol status, and if you have had any falls in the past year.
- Lifestyle – Let us know about the following as there is a chance it may play a role in your eye health: Your caffeine consumption, whether you play wind instruments, perform frequent inverted head positions in activities such as yoga, are a heavy weight-lifter, or have any significant restrictions in your diet.
Major Parts of the Eye Examination
 Visual Acuity. This checks your vision in the center, which is different from visual field testing (which also tests your peripheral vision). You will be asked to look out of your right eye first then left with your current glasses or contacts. If needed, pinholes will be put in front of the tested eye and you will be asked if this improves the vision.
Visual Acuity. This checks your vision in the center, which is different from visual field testing (which also tests your peripheral vision). You will be asked to look out of your right eye first then left with your current glasses or contacts. If needed, pinholes will be put in front of the tested eye and you will be asked if this improves the vision.
Microscopic Eye Examination. Your ophthalmologist will use a specific microscope to examine the front part of the eye (the cornea, lens, and the colored part of the eye called the iris), and the back part of your eye (your optic nerve and retina).
Checking Eye Pressure. Normal eye pressure ranges between 10-21 mmHg in most patients, and it could be measured with different devices. Eye pressure is unique to each person. Some patients may have glaucoma with an eye pressure less than 21 mmHg. Eye pressure more than 21 mmHg does not mean that you have glaucoma if other tests are within normal limits.
- Tonometer is the name of any device that checks eye pressure. The applanation tonometer comes close to the eye's surface after the eye has been numbed and measures the eye pressure. This is the most accurate tonometer and requires using an eye drop that makes your tear yellowish (for a very short period of time).
- Hand-held tonometers are portable hand-held devices that measure eye pressure and may not require numbing drops.
- A hand-held device will be used to check the thickness of the cornea (pachymetry) to better evaluate the eye pressure.
IMPORTANT
It is very important to request your medical records from your prior and/or current eye doctors and confirm that they have been received prior to your first appointment (or better yet, bring the records with you). These records should ideally include prior eye pressures, maximum eye pressures, prior surgery or laser procedures, prior testing (visual field, disc photos, or optical coherence tomography (OCT).
Meet Wills Eye Glaucoma Doctors


JOEL S. SCHUMAN, MD
Co-Director

L. JAY KATZ, MD
Emeritus Director

ELIZABETH DALE, MD

JASON FLAMENDORF, MD

LAUREN E. HOCK, MD


NATASHA KOLOMEYER, MD
DANIEL LEE, MD

LINDSAY MACHEN, MD

MARLENE R. MOSTER, MD

MICHAEL PRO, MD

REZA RAZEGHINEJAD, MD

MARY JUDE COX, MD

RACHEL NIKNAM, MD

JESSE RICHMAN, MD

GEOFFREY SCHWARTZ, MD

COURTLAND SCHMIDT JR., MD

ALICE WILLIAMS, MD

Gonisocopy (checking the drainage system). The drainage system is located where the colored part of the eye (iris) meets the cornea (the very front layer of the eye). The doctor uses a special lens to view the drainage system to determine if it is closed or open. In the closed type, the iris is very close to the cornea and covers the drainage channel. In the open type, the colored part is not close to the cornea and the drainage system is visible. This test helps differentiate between the two major types of glaucoma or glaucoma suspects: open angle and closed angle.

Dilated Eye Examination. Special drops may be used to temporarily enlarge the pupil so that your doctor can better view the back part of your eyes (retina and optic nerve).
Dilation drops take approximately 15-20 minutes to take effect.
They can last a few hours and may cause some light sensitivity and your vision to be more blurry (especially up close) during that time.
For more general information regarding planning your visit to Wills Eye Hospital, refer to our Plan Your Visit page.
