Uveitis Explained
Video Transcript
Uveitis Explained by J.P. Dunn, MD
Hi, I’m J.P. Dunn. I’m the Director of the Uveitis Unit in the Retina division here in Wills Eye Hospital, and I am here to talk a little bit about uveitis.
What is Uveitis?
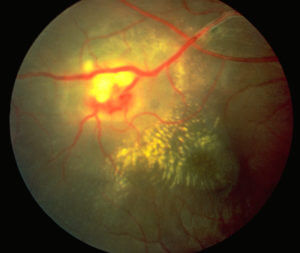
Uveitis is intraocular inflammation that involves are a very large segment of different diseases. Uveitis can occur in the front of the eye, in the middle part of the eye, in the back of the eye, can involve the entire structure of the eye. When patients are diagnosed with uveitis, it’s often very confusing. You can go to Google and look up uveitis and terrify yourself, because often the first thing you see is blindness.
Causes
Uveitis is very much like arthritis. There are many different types of arthritis - they can range from a mild annoyance to someone confined to bed from their arthritis. Uveitis is the same way. There is a whole spectrum of disease. Our goal is to try to find out:
- What’s causing the uveitis;
- What’s the most effective treatment for the uveitis, so controlling the disease while trying to minimize the side effects; and then
- Following the patients long-term to make sure the visual outcomes are as good as they can be.
When a patient comes in with uveitis, the very first thing we do is take an extensive history. A lot of uveitis can be diagnosed just based on a careful, full ocular examination and a good medical history. Clues to other diseases that are going on - things like sarcoidosis, inflammatory bowel disease, different types of arthritis, certain infections - all of those can be critical components of finding out what is going on in the patient's eye.
Evaluating a Patient for the Disease
So our first task when we evaluate the patient is to decide is this an infectious or noninfectious uveitis. Clearly the treatment for those is going to be very different. If it’s an infection, we are going to treat the patient with antiviral medications, antibiotics, anti-fungal medications. If it’s a non-infectious, uveitis then we have to decide what is the best treatment for that. And as I mentioned, uveitis can occur in the front, middle, or back of the eye.
Treatment
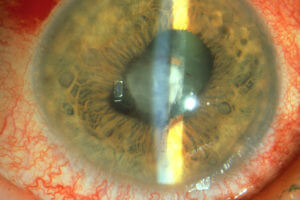
For many types of uveitis, anterior uveitis (or inflammation involving the front of the eye) is far and away the most common thing that was see. Anterior uveitis is often treated with steroid eyedrops. Steroid eyedrops can be very effective as anti-inflammatories, but they can cause problems. Steroids increase the risk of cataract, and they can increase the risk of glaucoma or they can worsen pre-existing cataract and glaucoma. So, there are certain cases where we need to work very carefully with the Glaucoma Service here at Wills or a patient’s other glaucoma specialist to manage their uveitis while not making their intraocular pressure (or causing their intraocular pressure) to go out of control.
In cases where we can’t use steroid eyedrops, sometimes we use other non-steroid anti-inflammatory agents. We tend to do this more for inflammation that is deeper in the eyes, or inflammation involving the retina, the choroid, which is the layer deep to the retina, for example. Those patients, when they need these so-called steroid sparing or immunosuppressive agents, have to be carefully evaluated to see if they are going to tolerate those medications.
Immunosuppressant Therapy
There are a number of different immunosuppressants that can be used. Each of them, as categories, has their own advantages and disadvantages, and we can always try and mix and match the patient’s medical condition with what would be the most appropriate immunosuppressive agent. As you’d expect from the name immunosuppressive, these are medications that suppress the body’s immune system.
A large part of uveitis is autoimmune disease. By that we mean think of the body’s immune system as getting confused and attacking its own cells. The classic autoimmune disease is rheumatoid arthritis. The immune system gets confused, it attacks the joints, the joints get red, swollen, damage to the structure of the joints. Again, that parallel between arthritis and uveitis holds.
So with uveitis, we have to try to figure out what’s going on systemically. Some of the medications that we use for immunosuppression to dampen down that overactive immune system may affect the liver, others may affect the kidney. It is important understand what the patient's underlying medical problems are. If they have renal disease, kidney disease or liver disease, they might not be good candidates for certain medications.
Immunosuppressive therapy is often long-term therapy. It's not usually indefinite therapy, but as a general guideline if we start immunosuppression on a patient, we may be doing that for up to two years. And that’s assuming 1. the medication works well, and B. it’s well tolerated. If medications don’t work or aren’t well tolerated, there are a number of other immunosuppressants that we can try.
I have a particular vested interest in immunosuppression because I take immunosuppressive medications myself. Shortly after I came to Wills, I had exacerbation of a long-standing genetic heart disease, and I ended up needing a heart transplant in 2014. And ironically the same medications that I use to prevent rejection of my heart transplant are the same medication that I often prescribe to treat ocular inflammatory disease. So, as I tell my patients, I literally get a taste of my own medicine on a regular basis in my clinic.
There are some patients that won’t need immunosuppressive therapy but need something more than just a steroid eye drop. These may take the form of steroid injections or steroid pills. Those, too, may have side effects. Steroid injections have the advantage of avoiding systemic side effects,, but some people don’t like getting a needle around the eye no matter how much we anesthetize the eye. Oral steroids have the advantage of treating both eyes in a patient who has bilateral disease, but oral steroids have many potential side effects ranging from relatively mild things like stomach upset or irritability, some difficulty sleeping, weight gain, acne, to much more serious problems like diabetes, high blood pressure and osteoporosis or thinning of the bones. In a patient who is treated with long-term steroids, we work carefully with the patient’s doctors to make sure that they are tolerating those medications well.
Some patients need surgery when they have uveitis. That surgery may be related to glaucoma that the uveitis causes or the steroid medications cause. It may be retinal surgery in patients who develop a retinal detachment or develop inflammation in the vitreous gel in the eye that needs to be removed. It maybe cataracts. They may have extensive scarring around the pupil that needs to be managed at the time of cataract surgery. That is what I do in my surgical practice. The only surgeries that I do are what are called complex or uveitic cataracts. So, patients that have had uveitis, that have scaring around the pupil, and that requires a special type of cataract surgery. Those patients also required particularly aggressive anti-inflammatory therapy around the time of cataract surgery to minimize some of the potential complications.
So that’s kind of an overview of what we do in uveitis. It is important for patients to remember that for perhaps up to 40% of patients with uveitis, we don’t know what actually causes the disease. We call that idiopathic uveitis, and patients can get understandably frustrated when they don’t know what the cause of the disease is. For many of those patients, we're able to reassure them is that we don’t know what’s causing the disease, but we know how to treat it, and we know how to manage the complications of the disease.
I think the most terrifying thing for patients who carry diagnosis of uveitis is they really don’t know what Uveitis is. As I said you could Google uveitis and think that you are going to go blind because that will be one of the terms that comes up quickly. Most uveitis, in fact, can be treated very effectively. It’s important that patients understand that they need in many cases long-term therapy, they need to work carefully with their uveitis specialist.
We have the advantage here at Wills that because of the multiple potential complications of glaucoma, of cataract, of retinal problems, that we have the full range of specialists here that treat any manifestation of uveitis that may come about - and that in some cases even includes low vision consultation for patients in whom we can’t restore very good vision. That fortunately is relatively uncommon, but it does occur.
Part of coming to Wills that makes it good for patients is not only the collaborative effort of all of the physicians here, but the fact of patients may be eligible for certain studies. So they get the opportunity to be treated with cutting-edge medication and treatment protocols that may not be available to them on the outside. We’ve had a number of patients that have taken part in clinical trials here, clinical trials that we do as part of multi-center trials sponsored by the National Eye Institute and other pharmaceutical company-sponsored trails. So patients have all the opportunities to get the very latest treatment for their uveitis.
And fortunately nowadays with all of the medications and all of the treatments we had offer, the prognosis for Uveitis is much better than it was many years ago. Uveitis is still one of the leading causes of blindness, but studies repeatedly show that one of the most important negative risk factors for patients with uveitis is delay in a referral to a uveitis specialist. Once patients get seen and properly treated, they can often do very, very well.
So, I would like to thank you for listening, my name is J.P. Dunn I am the Director in the Uveitis Unit in the Retina Division here at Wills Eye Hospital and I appreciate your attention.