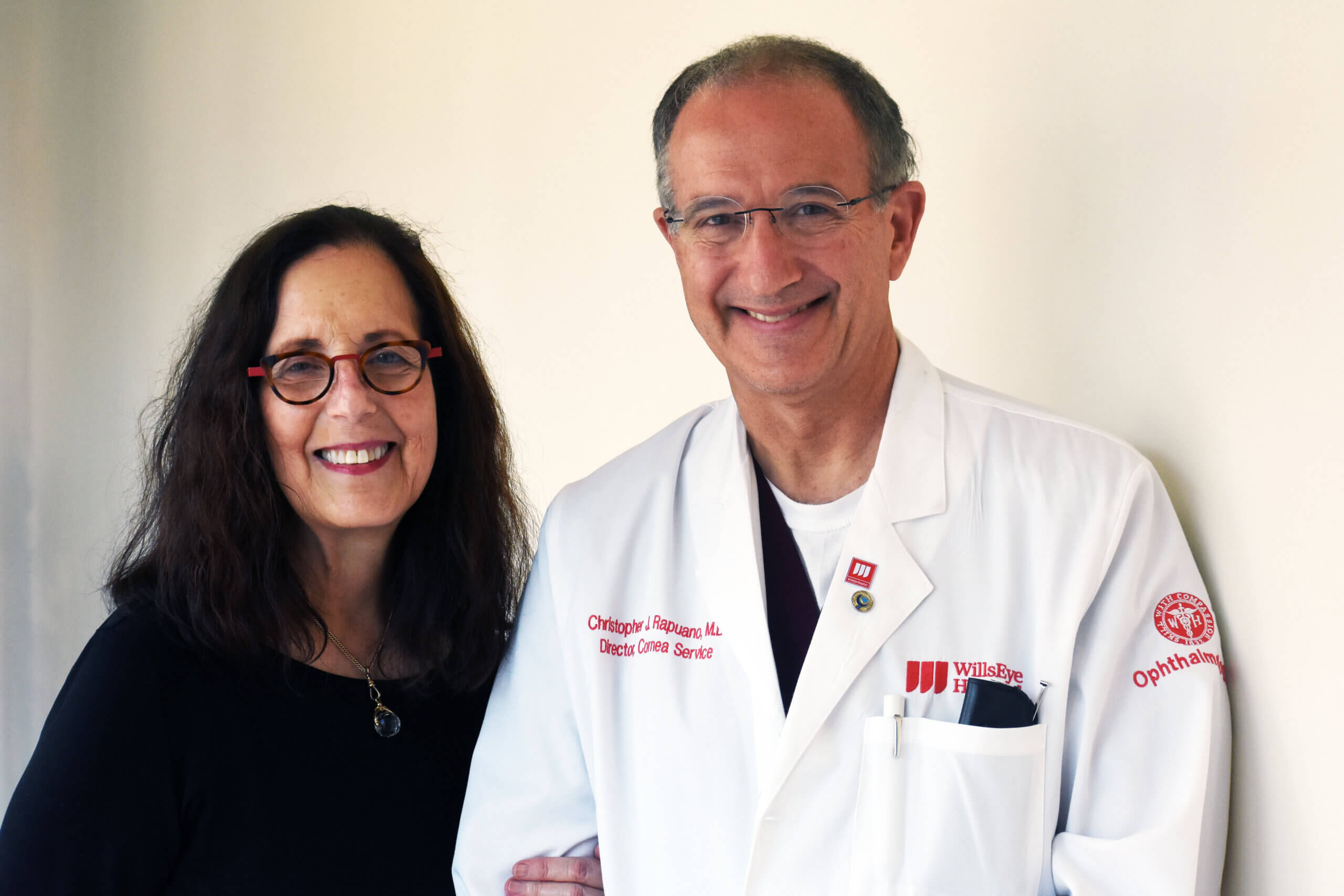
You'll receive expert, specialized care from one of the nation's premier academic eye hospitals.
I
You'll receive expert, specialized care from one of the nation's premier academic eye hospitals.
Established in 1832, Wills Eye Hospital is a renowned eye hospital and global leader in ophthalmology. Ours doctors and staff are focused on treating patients with eye disease and specialize in providing the best care and treatment for your eyes. From comprehensive eye exams to rare and complex vision conditions, our specialists ensure the best care that is customized for each patient’s need.
I
Established in 1832, Wills Eye Hospital is a renowned eye hospital and global leader in ophthalmology. Ours doctors and staff are focused on treating patients with eye disease and specialize in providing the best care and treatment for your eyes. From comprehensive eye exams to rare and complex vision conditions, our specialists ensure the best care that is customized for each patient’s need.