Wills Eye retina doctors are leading experts in the treatment of macular degeneration with the latest clinical trials and new therapeutic approaches for AMD.
Age-related macular degeneration (AMD) is a common condition affecting people age 50 years and older that is associated with central vision loss, which affects one's ability to read, drive, or see someone’s face if it progresses to more advanced stages.

CAUSES
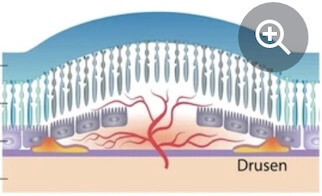
Age-related macular degeneration is a complex, degenerative condition that becomes increasingly prevalent with advanced age. It is typically found in people ages 50 years or more, although drusen sometimes can be seen in younger people. Family history is another important association, although simply having a blood relative with AMD does not necessarily mean or guarantee that one will definitely develop AMD. Other risk factors for AMD may be modifiable or controllable, including smoking, poor nutritional intake, and high blood pressure.
SYMPTOMS
Many people with mild dry AMD have little to no visual symptoms. Some people, however, will experience some side effects, including:
• Requiring more light to read
• Difficulty adjusting between dark and light conditions
• Mild blurring of vision
Occasionally, people may not be aware of these visual changes because their other eye sees well. Therefore, it is important to test vision in each eye separately by covering one eye at a time when checking vision.
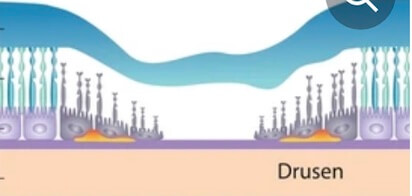
Dry AMD affects about 90 percent of all people with macular degeneration and is characterized by drusen.
PROGNOSIS: Most people with AMD will retain good central vision and the ability to read in their lifetime, although dry AMD may also gradually progress to an advanced form with atrophy of the macula, limiting central vision.
SYMPTOMS: Many people with mild dry AMD have little to no visual symptoms. Some people, however, will experience some side effects, including:
• Requiring more light to read
• Difficulty adjusting between dark and light conditions
• Mild blurring of vision
Wet AMD affects only about 10 percent of people with macular degeneration, yet accounts for the majority of central vision loss in those who have AMD.
PROGNOSIS: People with wet AMD will quickly suffer central vision loss if left untreated. While patients may progress to legal blindness, it is important to realize that AMD affects central vision – it typically does not lead to total loss of vision.
SYMPTOMS: Patients with wet AMD often have pronounced symptoms, including:
• Rapidly progressing loss of central vision, typically over days to weeks
• Visual distortion
There is no treatment available yet that can either halt the progression or recover vision loss from dry AMD. Based on epidemiologic studies, certain lifestyle and nutritional changes may be beneficial.
In the past, laser-based therapies were used to target the abnormal blood vessels that cause wet AMD. However, the laser burns typically resulted in scarring and damage to central vision. Fortunately, there are now anti-vascular endothelial growth factor (anti-VEGF) medications available for the treatment of wet AMD. These medications, injected into the eye as an office-based procedure, are currently the preferred therapy for wet AMD due to their unprecedented efficacy. They represent the first therapy that has ever been clinically proven to help improve vision in a substantial proportion of patients with wet AMD. Timing is important, as earlier identification and treatment of wet AMD is associated with better visual outcomes.
Wills Eye Retina specialists are in the forefront of research efforts, participating in multiple clinical trials to investigate new forms of treatment for macular degeneration and a variety of other retinal conditions.
• Longer-acting Pharmacologic Agents
• Port Delivery System
• Gene Therapy
• Anti-inflammation
• Cell Based
• Genetic Screening